A Cause for Unexplained High Glucoses (UHGs) on a Pump
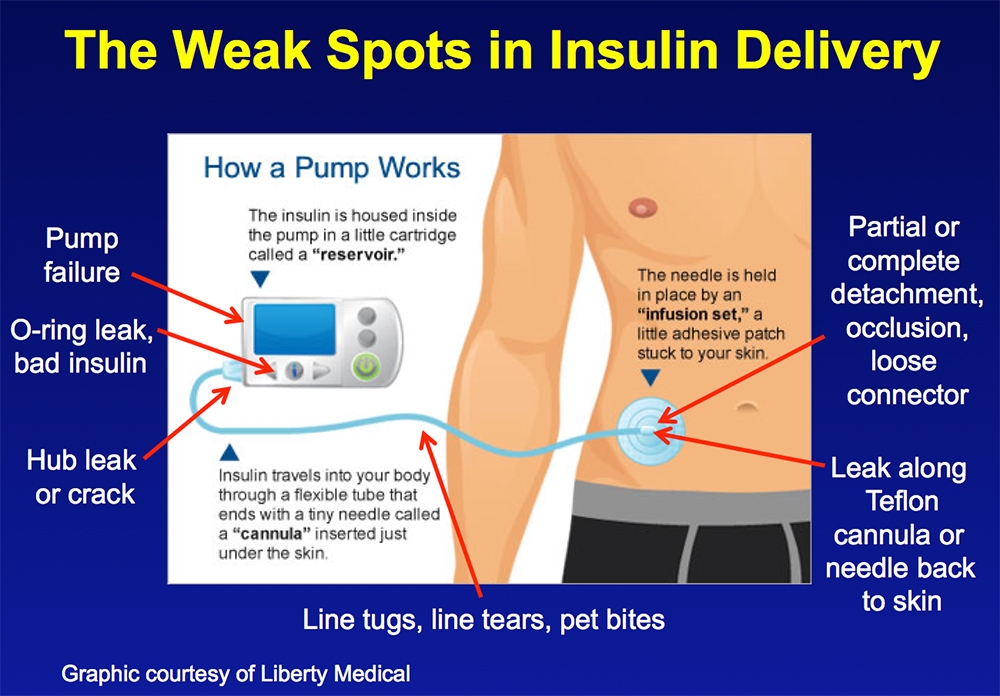
Today’s infusion sets offer many improvements and options, yet reports and blogs suggest issues with infusion sets are widespread. Only a handful of studies have directly looked at this problem.1 Infusion set leaks and failures create random unexplained high glucose values (UHGs). They also make up most phone calls to manufacturers and end up being a common reason that people stop wearing a pump. The Weak Spots graphic shows all the ways you can lose insulin, but nearly all UHGs arise from the infusion set, NOT from pump failure or having a “bad infusion site.” So set detachments and leaks along a Teflon cannula or steel needle are the most common sources for UHGs. Go Here if you are unfamiliar with an abbreviation or term.
Infusion set failure represents the great white whale on your quest for good glucose readings. Lurking just below the surface, it bumps your glucose high and sets you up for failure. Infusion site failures are a common source for UHGs compared to “bad infusion sites” or “bad insulin”, two extraneous causes that often get the blame. Don’t be Ahab – catch the great white whale!
Four research studies have looked at initial failure rates when Teflon sets are inserted with an auto-inserter. Initial failures ranged from 3.2%2, to 8.9%2, to 10%, to 15%3. Among 1,142 German pump wearers, 72% of those who used an auto-inserter reported that it failed to work ~10% of the time.4 Set failures average 0.3-2.2 times/month for 2-3 day set use. In a review of a head-to-head comparison of two current infusion sets, 19% of both infusion sets required unexplained catheter replacements after insertion. Dr. Eric Renard, the main author, stated, “Fixing this weak aspect of CSII [insulin pump therapy] becomes crucial while moving toward closed-loop insulin delivery.”
If you’re on a pump, you probably use the infusion set brand that you started with, one recommended by your doctor or CDE, or one sent to you by the pump manufacturer. You probably haven’t given it a second thought since starting. The infusion set often doesn’t come to mind as a significant source for glucose control problems. Infusion set problems, unfortunately, cause far more hyperglycemia for those whose glucose levels are highest.
Having more than one infusion set failure a month raises the A1c.
Set failures can be hard to recognize. Pump wearers often change their infusion set and site any time they encounter unexplained high glucose readings. This is often done grudgingly without fully realizing that this intermittent problem is coming from their infusion set.
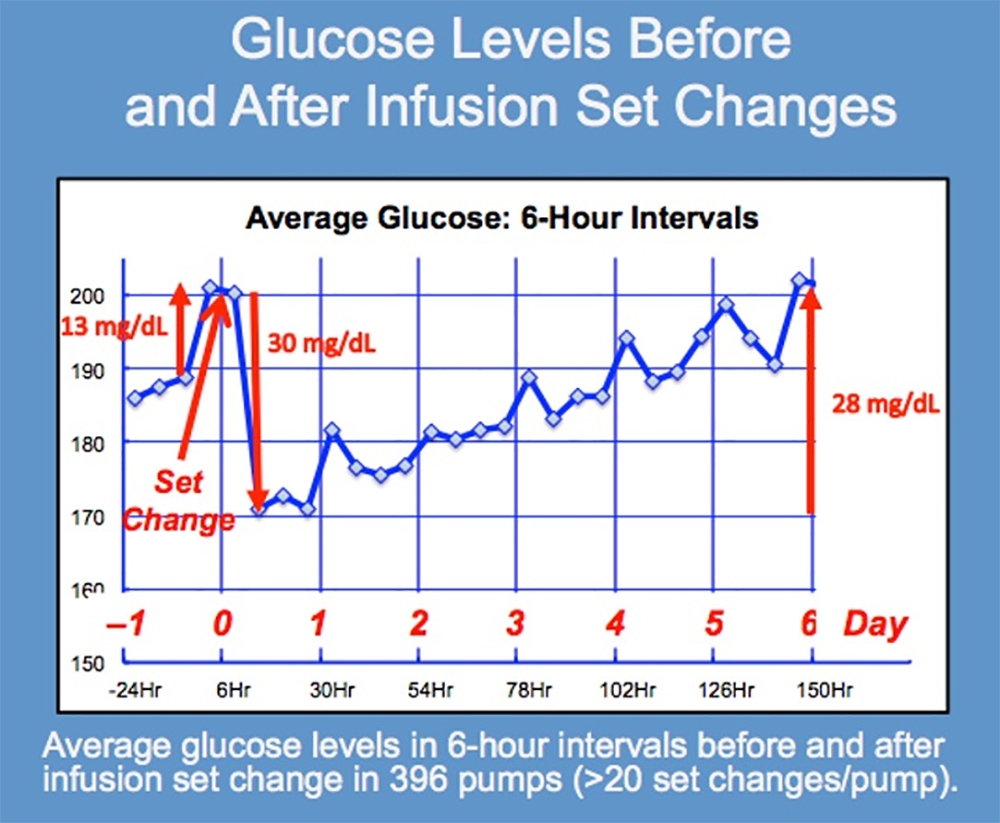
This graph of unpublished Glucose Level data from the Actual Pump Practices study shows average glucose levels in 6-hour intervals beginning one day before a person changes their infusion set up to 6 days afterward. There was an average of 20 infusion set changes per person among these 396 pump wearers.
Note the very large 30 mg/dL fall in average glucose levels 12 hours after infusion sets are changed. This drop occurs as insulin delivery again becomes fully reestablished. Note also that glucose levels immediately begin to rise as infusion set problems gradually reappear.
An alternate explanation could come from decay in insulin activity over time within a pump reservoir, but John’s experience with thousands of pumpers does not agree with this theory. He has seen many pumpers who have UHGs suddenly have this problem disappear once they start anchoring their infusion sets. He and many of his patients wear infusion sets longer than 3 days with no loss of control.
To evaluate your current infusion set, answer these questions:
- Do you have to change your infusion set before 3 days of wear?
- Does your glucose often rise on day 2 or 3 of set wear?
- Do you often have UHGs (unexplained high glucoses)?
- Do some highs only correct after you change your infusion set?
- Do correction boluses sometimes not work as they should?
- Do unexpected highs appear right after changing your infusion set?
- Do sites sometimes not work, or have you been told you have “bad sites, scarring or poor absorption”?
Assume your infusion set has failed any time that you experience 2 unexplained highs in a row that don’t respond to correction boluses or remain high for over 5 hours on your CGM. Give an injection immediately to bring the glucose down. The dose will often be higher than expected due to the prior loss of basal insulin. Then change your site, infusion set, and reservoir.

Teflon or Steel?
Teflon cannula infusion sets, while purportedly more comfortable than steel sets, are not more comfortable but are often to blame for infusion set failure. Failures with Teflon sets can occur at any time, are occasionally seen right after insertion, but are most common on day 2 or 3. Quick-sets are especially prone to failure due to the pinch, twist, and pull motion used to disconnect and reconnect the line directly above the Teflon cannula when bathing or any other time the pump is disconnected.
| 3.3 Infusion Set Options | |
|---|---|
| Steel | Polymer |
|
|
Set failures typically do not trigger an occlusion alarm because they don’t block the tubing but result from a slow leak of insulin along the Teflon cannula to the skin surface or a faster leak when the set completely detaches. In a recent study of pigs who had 30° or 90° Teflon infusion sets changed every two days over two weeks, the 30° slanted set reduced inflammation significantly (9.1 versus 14.3 square millimeter, p < 0.001) and the thickness of inflammation (0.7 versus 1.2 mm, p < 0.005) at the infusion site compared to 90° sets, and they also had a wider distribution of insulin for better absorption.5 This may minimize site issues.
While testing your pump settings to optimize them, we highly encourage you to use a steel set like the Medtronic Sure-T, Tandem TruSteel, or Contact Detach for Luer lock pumps. Their short 6 mm fine gauge needle under the skin is as comfortable as Teflon, and more importantly, dependable, eliminating the particularly infuriating variable of set failure. To switch to steel, you can usually contact your distributor. On occasion, a new prescription is needed.
Many people safely ignore the “2 days of use” recommended by manufacturers for steel sets, even though there is no documentation for this. Among 534 pump wearers in the U.S., Teflon sets were used for an average of 3.4 days and steel sets for 3.7 days.6
Infusion Set Tips:
- Use an infusion set with a high success rate: 6 mm steel (or a shorter one, if available). The tubing connector for steel sets is about 4” away from the insertion. The remote detachment allows an IV3000 or Tegaderm adhesive to be placed on top of the site with most of the adhesive placed over the tubing. This is done only one time after inserting a new set.
- Always anchor the infusion line to eliminate any movement of the needle or cannula from pump drops or tugs. For 30° or 90° Teflon sets, always place a short length of 1” Durapore or similar tape over the line about 3” away from the cannula. Replace the tape each time after bathing or detachment.
Goal: Allow no more than one infusion set failure a year.
For more information about infusion sets, see our Infusion Set Comparison page or read Chapter 15 of Pumping Insulin.
Next, check your pump settings.
1 Heinemann L, Fleming GA, Petrie JR, Holl RW, Bergenstal RM, Peters AL. Diabetes Care. 2015; 38: 716-722.
2 Renard E, Guerci B, Leguerrier AM, Boizel R. Analysis of “Randomized Cross-Over Study Comparing Two Infusion Sets for CSII in Daily Life” Diabetes Technol Ther. 2010;12:769-773.
3 Patel PJ, Benasi K, Ferrari G, et al. Diabetes Technol Ther. 2014;16:15-19.
4 Heinemann L, Weber D, Kaltheuner M, Scheper N, Faber-Heinemann G, Reichert D. Abstract #994-P. American Diabetes Association 73rd Scientific Sessions, Chicago, IL, 2013.
5 https://drc.bmj.com/content/7/1/e000881
6 Walsh J, Roberts R, Weber D, Faber-Heinemann G, Heinemann L. J Diabetes Sci Technol. 2015, Vol. 9(5) 1103–1110.

My infusion set falls off when I am sweating what can I do to prevent this from happening?
Hi Donald! Infusion set failures are no fun! Try these tips for solutions for sweating with infusion sets and CGMs.
After 26 years of being on an insulin pump the last year or two has seen a dramatic rise. I was doing so well and take excellent care of myself but this is unbelievable. I have an almost 100% initial failure rate; yup, EVERY…. SINGLE….. ONE is failing. After changing sets I often get skyrocketing sugars. When I take it out it often tends to bleed. Just because I change it doesn’t mean it gets fixed. Often I need to put it 2, or even 3 to get “good luck”.
It doesn’t matter where I put it in. Tried back of arms and legs too where I might be giving shots as well to put them in it always fails, high sugars after every one of them. The last month and a half or two pretty much every single insertion fails. Had a minimed pump back in 1995 which went to Medtronic. Am due for a new one and am considering switching. Although it worked so well for so long any pumps out there with better luck and more reliable sets?
Hi Attilio,
Sorry to hear about the set failures. Please let us know more about what happens:
1. Which infusion set are you using?
2. Let us know about rotation. Do you normally rotate sites over the whole abdomen, above and below your beltline, on the flanks, upper buttocks, etc.?
3. How high and how soon do your BGs rise after putting in a new set?
4. After inserting a “good” set, are your BGs then relatively normal?
5. Are there any other signs of a failed set such as a damp adhesive, or liquid or the odor of insulin on the skin?
Thanks,
John
I don’t see that Attillio replied to your questions, but I will! I am have the same problem, been a pump user for 4 years. Everything was great! 5.6 A1C with pump and low carb diet. All of the sudden a year ago starting having this problem. Using the Tandem T Slim, was originally on the Auto soft 90, then went to Auto Soft 30, then went to Tru Steel – got them to send me a new pump. None of these changes have worked. Currently using the Verisoft. Currently changing the site every day, but as you mention it takes hours to get the problem corrected, not to mention my infusion set and insulin usage has increased dramatically. My A1C is now a 6.3 and I feel like I am dying a little bit each day because of it. I tried to go back to manual injections, but the lows were unbearable. I am trying to get an appointment with a new endo, but this also takes time. I left my last one because she and I did not see eye to eye on diet and I felt she was belittling me even though I had great A1C’s. I did not see this problem coming and I am at wits end. I also tried the Omnipod – but could not get an average any lower then 160. Any advice or am I just crazy and missing something crucial?
Shanna, an A1c of 6.3 is excellent, meaning your daily dying is REALLY SLOW!
From your note, it’s unclear why you are changing our infusion set daily. Please tell us more.
Despite Dr. Bernstein’s “advice,” I am NOT a fan of low-carb diets because of their increased mortality (see pages 49 to 52 in the 7th ed.). I’m hale and hearty after over 72 years of using insulin with a moderate to high healthy carb intake. ;–))
Would you recommend at pump change an increase in basal or a upfront bolus to cover the time it takes for the pump to re establish full control?
I sometimes take 2 units since I find the pump needs two hours to re-establish control were i miss 2 hrs of basal, the bolus also works equal to the amount of basal issued.
A 2 unit bolus would be appropriate if you consistently have your glucose rise when you change infusion sets. A basal adjustment would take longer to have an effect. You might consider a smaller bolus if the rise in glucose is not consistent.
If you are using a Teflon infusion set, they are prone to silent occlusions. Becton Dickinson researchers looked at this carefully. A silent occlusion occurs shortly after insertion when tissues around the cannula compress it and reduce the flow of insulin. The glucose then rises but the pump does not alarm, hence the “silent” in front of occlusion.
FYI, steel sets don’t do this, are easier to insert, and are generally worn longer than Teflon sets. Might be worth a try!
A Pumper’s Question:
“I have a Tandem pump and use the Auto Soft 90. About one in eight or ten times there is a failure resulting in very high glucose and I have to change the infusion set. The main cause is the adhesive backing pulls up when I disconnect from the insertion device. I have told Tandem about this and evidently, they don’t care. I never had this problem with AccuChek infusion sets.
Can I change to a more reliable infusion set made by another company?”
Response:
Infusion sets have always been the weak link for insulin pumps. As you’ve noticed, some auto-inserters don’t always fully detach from the set when the spring retracts. This leads to a kink in the cannula or insulin leaking back to the skin along the cannula. Unfortunately, all pumps have a proprietary connection to the pump body, so the Auto Soft is the only similar set that I am aware of for the Tandem.
A quite reliable alternative is the TruSteel 6 mm set. It’s easy to insert, much less likely to fail, has a flat profile on the skin, and is usually worn longer than Teflon sets. I cover the insertion site and part of the infusion line with an IV3000 or Tegaderm adhesive, after removing the adhesive at the connector base about 4 inches away. This over-bandage keeps the set securely connected to the skin for the duration of wear. You can then easily detach for showers, etc., and with the connector base unattached to the skin, it provides a longer infusion line. Your goal is to have no more than one infusion set failure a year. Might be worth a try!
You learn a lot after 39 years on a pump! ;-)
John Walsh, PA, CDTC
I use the Medtronic 630G and every single set change of Cannula & Reservoir gives me 6 to 8 hours of very High Glucose readings. I have to increase the Basel up to 5 units in increments of 30 minutes depending on the glucose readings from my Dexcom. My A1C has increased from 6.9 to 7.7. I have changed sites a bunch of times but to no avail. Maybe I might have “LIPODYSTROPHY”. Any suggestions?
Hi Fara,
Lipodystrophy is a very uncommon reason for very high glucose readings after set changes. I assume your set change does not take a couple of hours and you are priming your infusion line and have insulin visible on the cannula tip?
Was this happening when your A1c was 6.9%?
Is there any other reason for the higher A1c, such as an increase in weight, decreased activity, or change in diet? If there is another reason, you may need to raise your basal or lower your CarbF (iSF).
With the higher A1c, your basal rate high be too small and the time to change the set may send the glucose higher. Check in your pump history to verify that your basal rate makes up at least half of your total daily insulin dose. If not, consider raising your basal rate, which you may need to do anyway with the higher A1c.
Another option is to change to a different type of infusion set to see if that corrects the problem.
Good luck,
John
This is a weak answer. People who have used a pump and all of a sudden have unexpected high bg readings after a set change myst be common. Something has to be wrong… very wrong. 50 percent of the time my infusion sets don’t take… They used to but now don’t. Steel cannula 6mm or 8mm all the same. Unbelievable to say the least. Something has changed and not in a good way.
I had had set failures before but not very often. The recency of your problem sounds very familiar. Not tried steel yet though.
I agree with you Paul. I think the manufacturer’s sales have increased dramatically in recent months and in “tandem” with increased sales is a decrease in quality control. I’ve only been on Tandem for 7 months using TruSteel both 6 and 8 mm, and the number of infusion set failures I have experienced is totally unacceptable. It is our HEALTH at stake! And our pocketbook, those things are expensive! I am just about ready to quit this scene.
In the care of hundreds of pumpers using the 6 mm TruSteel, BGs rising when the set changes DOES happen but is rare. With the TruSteel set, I encourage not using the second adhesive for the connector, but removing it and always placing a 3″ length of 1″ Durapore tape over the line a couple of inches away from the set. This reduces movement on the steel needle from kinking that sometimes occurs between inserting the infusion set and tacking down the connector adhesive. This ensures proper anchoring with no loop between the anchor and the set.
I have not noticed a loss of quality in manufacturing these sets. Remember, if one set seems to cause problems, always try another set. This ends the problem if the set is the cause.
In the Actual Pump Practices Study, the average glucose rose higher for each day of use. This suggests loss or leakage of insulin. Nearly all participants used Teflon sets. If the glucose is higher toward the end of set use, this may contribute to the glucose being higher after changing sets. Your liver reads insulin, not glucose levels, and will release more glucose as the glucose approaches 140 mg/dl. Good anchoring on the cannula might help.
Per Paul’s “weak answer, ” an answer becomes much clearer when you clearly explain the problem and its circumstances.
I’m on Tandem for about 6 month. I’m absolutely shocked because every single infusion set is failing and /or giving/ leaving me with horrible site and scar on my body. I have tried all the types of infusion sets including trusteel. Every single Trusteel fails in 6-8 hours. I used before Metronic pump and never had a problem with infusion set…ever. But Unfortunately Metronic Guardian glucose monitor sensors are are complete failure. They simply don’t work. So I switched to Tandem with Dexcom and I’m facing disaster now. Dexcom is great. Tandem pump is good too but it doesn’t matter how good pump is if infusion sets doesn’t work. I’m greatly disappointed and after being on different pumps since 2012 I went back to manual injections. Back in time I used Omni Pod and loved it. I would love to go back to Omni Pod 5 again but not sure if its possible because I already got Tandem. Each pump had 4 year warranty for the insurance to replace to different pump. Please let me know how can get away from Tandem to OmniPod 5.
Thank you
I am so grateful to have found this article. About the past month, I have been ready to lose it, with multiple styles of teflon-cannula sets failing. Now I know to switch to steel! TYVM!
I have Medtronic 670g starting last fall the first day I put in a new site and I use the quick sets my sugars stay actually low then within about 13 hours it slowly goes up no matter what I do n more n more I’m ending up in ER with sugars almost 600 after I get an iv drip get it half way down they have me change the site then I’m good for a day n this is happening more n more i get told it’s from being a type one for so long that I have I have a lot of scar tissue n I starting to get scared I’ve been a diabetic 37 years and just like that having issues I eat a very low carb diet under 50 carbs a day I’ve always been a larger person am I weight is very steady I am so routine I don’t get it and I’m scared
Hi Cris, very sorry to hear about the infusion set issues. FYI, the Quick Set is known for its high failure rate. Companies with a new infusion set always use the Quick Set as their comparator! Try Medtronic’s Sure-T-6 mm 30″ set. This steel needle has a finer gauge, a lower profile, is easy to put in by hand, and is far more reliable as long as you anchor the line. If you’ve always had problems with the Quick Set (more than one failure a month) definitely replace it. If you use the inserter, its spring can get weak and cause failure at insertion, which sounds like the problem you are having. The insertion device should be replaced once a year. But be aware, I NEVER use Quick Sets with my patients.
Scarring can occur, but this is a misdirection that all the pump companies use. Avoid hard nodules under the skin with the Sure-T sets for awhile and this should resolve.
Also, correct highs once. If a second bolus fails to correct the glucose, take an injection by pen to correct the glucose AND your mission basal insulin. Then immediately replace the infusion set, the WEAK LINK in pumping.
I do not recommend low carb diets. Always better to eat a healthy, balanced diet! Use the Pump Settings Tool to check all your settings.
If weight or excess appetite is an issue, talk with your clinician about getting on a GLP-1 like Ozempic or Trulicity. Although approved for Type 2, they are often an excellent solution for Type 1s with extra weight.If you crave sweets, let me know.
If you are not on an automated insulin delivery device, switch to the Tandem/Dexcom Control-IQ or 770/Guardian AutoMode ASAP.
Gear your fear into finding solutions!
John
I feel like I have finally found a place that speaks to our experience. We’ve been on a pump for a year now only Tandem and after trying soft cannulas for sometime we finally switched to true steel. I’d say it’s better but it’s not best and we have many failed sites like right now. Just had a great 2-3 days I hated to change it. New site and it’s not working as we’re currently high ⬆️. So changing it again. Super frustrating as at times we burn through pumps!! When a site works we are in range. But with so many fails it’s extremely hard to keep his A1C in control. It’s a great option I hated pens but we really need it to work better.
Many times, after inserting a new infusion set, I noticed that insulin was coming out at the top side, rather than being pushed under the skin as needed. I’ve went into slight DKA in the past because I didn’t notice the leakage before the blood sugar spiked to a really high level, say 400 to 500.
I have in the past and still do when needed, put a piece of tape across the top part of the canula and many times thos helps correct the issue. Are there other things that can be done to keep the back flow from occurring? I use medtronic infusion sets. I’ve tried both 6mm and 9mm and both have had the same issue.
These things aren’t cheap even with insurance and I hate to have to throw one away and put on another.
Now, especially since our insurance only allows up to 3 boxes instead of 4. The 4th box worked great for such emergency cases, and to go to back ups. Now we don’t have that freedom along with more money spent.
Any help here is greatly appreciated.
Del, leaking from the top, sounds like a Teflon infusion set, and 6 or 9 mm means it goes straight in. Let me know if this needs to be corrected. If the set is Teflon, 6 mm Sure-T steel sets will resolve this annoyance. They are easy to insert and disconnect about 4 inches away from the set, allowing it to be anchored with an adhesive over the top or a 3″ piece of Durapore tape across the infusion line a couple of inches from the set. Let us know if this solves the issue. John
I’m wondering how people have found Trusteel sites with movement and activity.
I do massage therapy and am apprehensive about how well the steel needle will move with my body.
I am relatively slender and don’t have a lot of real estate for infusion sites. I typically used my thighs but my endo recommended switching to my abdomen and flank.
Can anyone offer feedback on how the Trusteel held up to activity, such as yoga or lifting weights? Did you notice the needle during movement? If so, did this affect absorption or cause the site to fail?
I know everyone’s body is different, I’d just like to hear from other T1Ds about their experiences.
Good to hear I’m not the only one struggling with the Tandem Autosoft 90s. I was starting to think I was crazy or doing something really wrong…
Also, wondering if anyone has any insights into why the Tandem sites have a (significantly) higher fail rate than other companies despite same supplier?
Tandem has such a beautifully designed algorithm in the Control IQ. It’s a huge disappointment that the supporting components don’t allow us end users to really experience the full benefits. When they work, my numbers are consistently under 10.0 (180) and easy to manage but I spend weeks on end rollercoastering and doing manual injections to avoid DKA due to failed sites. I average going through 7 infusion sets each site change, which makes me dread changing a good site and stretch it to 9+ days before rising BGs force me to change.
I have been on Tandem for 5 years. Frequent set failures, I have tried try steel and they are completely unreliable for me, I end up moving the needle and taping it down multiple times. I don’t know if my body is reacting to the steel tip. No occlusion warnings. I have been diabetic for 50 years and I am so frustrated I may go back to injections.
Hi Dan, my apology for the late response. Chapter 14 of the 7th edition has information on reducing set failures. It helps to have more information on what causes the “failure,” such as rising glucose, skin issues, or ? Inappropriate pump settings can mask as set failure. Have you found a solution?