When a pump or bolus calculator (BC) inaccurately measures residual bolus or short-acting insulin (SAI) activity, hypoglycemia can happen due to insulin stacking. Insulin stacking occurs when two or more bolus doses overlap and are working at the same time.
Go Here if you are unfamiliar with an abbreviation or term.
The risk of hypoglycemia substantially rises when someone enters a short duration of insulin action (DIA) or active insulin time (AIT) into a Bolus Calculator. Short DIA times hide insulin that is still actively lowering the glucose. The flawed dose logic used in current insulin pumps, BCs, and many AIDs can also generate excess insulin stacking. Many give a full bolus for all carb intake regardless of how much IOB is left. Even AID systems like those in the 670 and Loop/OpenAPS AID devices allow entry of short and risky DIA times.
Short DIA times and poor IOB accounting cause hypoglycemia.
Duration of Insulin Action
The measurement of IOB itself is determined by the DIA or AIT setting entry. The DIA time tells the pump how long a bolus of short-acting insulin should actively lower the glucose in your body. A correct DIA time is crucial because it ensures accurate accounting of IOB, minimizes insulin stacking, and enables more precise bolus doses.
There is much confusion about DIA. The DIA time defines how long a bolus continues to lower your glucose. This is a fixed property of the insulin that you use and does not change. Apidra, Humalog, and Novolog have identical DIAs of 5 to 6 hours. Three research studies have compared DIA between children and adults and found no difference.
Pumps and most Automated Insulin Delivery (AID) devices have a setting to specify DIA or AIT, except for Tandem’s Control-IQ that uses a preset and safer 5-hour setting.
Your Bolus Calculator uses the DIA to measure how much insulin from previous boluses remains actively lowering your glucose after 1 hour, 2 hours, etc. A short DIA hides IOB, and the resulting insulin stacking causes meal and correction boluses to be larger than you need. If you never give boluses within 5 hours of another bolus, you don’t have to bother with the DIA or IT setting because insulin stacking will not be an issue. Unfortunately, in the APP study, 67% of all boluses were given within 4.5 hours of another bolus, so overlapping carb boluses for most people are common.
Increased activity increases insulin sensitivity in muscle and other cells and lowers the glucose independently of insulin, making insulin appear to be “faster.” But it does not substantially change the insulin’s total glucose-lowering time or DIA. For example, a child might have gym class right after lunch and become hypoglycemic. Parents and clinicians might be falsely impressed by how “fast” the child’s insulin works. However on closer examination, they might realize that it would be better to cover only a portion of thee child’s lunch carbs because the remaining carbs were needed to cover their gym activity.
Pump users, clinical trainers, and clinicians, especially pediatricians, frequently set the DIA time too short. Short DIAs are often used as a “quick fix” to have the BC deliver larger bolus or injection doses when the real problem comes from undercounting carbs, having CarbF or CorrF numbers that are too large (making boluses too small), or having basal rates that are too low.
Short DIA times mask erratic insulin stacking and often lead to erroneous alterations of other pump settings, becoming a significant source for unexplained hypoglycemia. Rather than shortening the DIA setting to fix high glucose levels, always look for and fix the real problem.
| 7.8 How to Get an Accurate Bolus and Avoid Lows |
|---|
|
Tip: Set your DIA time to the actual working time for short-acting insulins like Novolog and Humalog. A good starting point is 4.5 to 5.5 hours for an insulin pump or BC, and between 5.0 to 6.0 hours for an AID. See pages 80-82 of Pumping Insulin, to learn more about DIA.
Careful! Some BCs recommend full carb coverage regardless of your IOB!
The DIA time has the most significant impact on IOB accuracy, but BCs also introduce insulin stacking by how they improperly handle IOB. Almost all pump BCs, some AIDs, and a few meter and phone apps recommend giving a full bolus for all carbs regardless of how much excess IOB is present.
It’s easy to see that carbs should not be fully covered with a bolus when IOB exists. If you have 5 units of excess IOB after playing tennis and your glucose is 120 mg/dL, today’s pump BCs ignore the 5 units of IOB and give a full bolus for all the carbs you enter into your BC.
Box 7.8, modified from page 85 of the 6th edition of Pumping Insulin, shows how to calculate an accurate bolus yourself. To avoid insulin stacking, subtract IOB for any correction and carb bolus/injection an hour and a half or more after your last carb bolus or injection.
Correction Boluses and IOB
When you take a correction bolus for a high glucose 2 or more hours after a meal, there is little or no carb digestion remaining to counterbalance any residual insulin action. Here, any IOB that remains will be lowering your glucose. Excess IOB needs to be covered with carbs any time the IOB is greater than the units required for a correction bolus.
Excess IOB can arise if correction boluses are too large, following increased activity, or when you give a larger-than-recommended bolus to rapidly lower a high glucose. Additional carbs are then needed to offset the excess IOB, as calculated in the Right Number of Carbs for a Low. This guidance provides the grams of carb needed to treat the low glucose. It is determined by your weight plus any extra carbs you need to cover excess IOB.
On an AID, basal delivery will have been reduced or stopped before the glucose goes low. Here, fewer carbs are typically needed to treat a low glucose. Always check your IOB, though, as this is what is driving your glucose down.
Measuring IOB After a Meal
Measuring IOB after a meal is slightly more complicated. For up to two hours after a carb bolus or injection, it is difficult to measure the activity of this insulin against the digesting carbs that raise the glucose. During this period of uncertainty, sometimes referred to as a “lockout time” or “dessert time-out”, you would typically cover additional meal carbs or an unplanned dessert fully. For most people and most meals, this uncertainty lasts for 1.5 to 2 hours following a carb bolus. Once digestion uncertainty passes, subtract any IOB above what is needed for your glucose from a carb bolus.
When the glucose is below your target glucose, some BCs appropriately recommend taking all of the excess IOB out of any carb bolus being given. Other BCs only remove enough of the excess insulin to raise your glucose back to your target. On the Omnipod pump, the user turns on a “reverse correction” option (aka, smart-thinking option) that subtracts some of the excess IOB from carb boluses once the glucose goes below the target glucose.
Unfortunately, current BCs do not tell you how many grams of carbs you need to prevent a low glucose. A smart BC would tell the wearer exactly how many grams of carb they need to prevent a pending low glucose when IOB is excessive. Lacking this guidance, users often overtreat low glucose readings. Check out the Right Number of Carbs for a Low to learn how many carbs you really need.

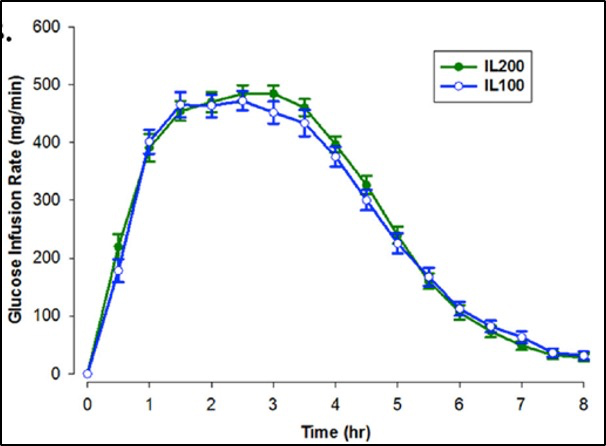
It’s nice to see an article addressing the shortcomings of modern pump therapy and the laziness of healthcare advisors trying to force the pump to make up for their inability to address underlying causes. There are too many healthcare advisors that are completely ignorant to the functioning of the technology they are pushing on us as the answer. One thing that constantly drives me crazy is that IOB is being calculated linearly! Obviously the action of insulin as graphed indicates that it’s not a linear burn, this seems like a huge factor worth considering when stacking insulin doses, which aside from user input is extremely common with current pump systems! I am so tired of my endocrinologist telling me auto-mode is going to fix all my problems while being totally ineffective at addressing the obvious problems I’m having with insulin stacking and incorrect carb ratio and correction factors (the same factors that drive the automode input!). I guess I’ll just have to take matters into my own hands if I want relief.
H, Chapter 8 in the 7th edition of PI details your righteous complaint. Some AID systems measure DIA linearly, but most use a curvilinear approach. DIA time is a more critical issue for accuracy. Still, ALL of the settings, including the TDD, CarbF, CorrF, basal rate, and DIA, have significant imprecisions detailed in that chapter and subsequent chapters. How to correct these are described in detail. Get the 7th edition for significant relief!!!