by John Walsh, PA, and Ruth Roberts, MA.
With Covid-19 everywhere, new variants spreading fast, and vaccinations at an early phase, a facemask remains your best defense. Also important, of course, are social distancing (more than you’d think), avoiding super-spreader Covid parties, and hand sanitizer and washing. Is there anything else you can do to strengthen and defend yourself?
There is. Over-the-counter treatments like vitamin D, famotidine (Pepcid, ~$10 for 60 tablets), zinc with quercetin, and vitamin C show real promise for significantly reducing damage during a Covid-19 infection. They strengthen your immune system, limit viral entry into cells, and reduce viral multiplication. Several promising prescription medications with anti-viral activity are undergoing testing. These include the diabetes medication Januvia (sitagliptin, ~$475 for 30 tablets). Januvia’s anti-viral activity is shared by an over-the-counter herb called berberine ($21.95 for 120 1,200 mg capsules), also used for diabetes. Easy availability, generally low prices, and safety make these agents especially attractive for personal use.
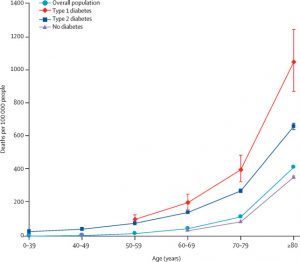
Diabetes requires extra protection against Covid. In an August 2020 article in Lancet, researchers evaluated Covid deaths among people with Type 1 and Type 2 diabetes among 61 million people in England. Mortality was twice as high for people with Type 2 diabetes compared to those with no diabetes. For people with Type 1 diabetes, mortality was even higher at 3.5-fold compared to similar non-diabetic adults. Fig. 1 shows these risks Fig. 1. The bottom line shows people with no diabetes, the top line those with Type 1 diabetes, and the next line below those with Type 2 diabetes.
This list reviews supplements and medications that impact Covid-19 outcomes:
- Vitamin D: Higher blood levels of vitamin D are strongly associated with less severe disease and lower mortality with Covid. Vitamin D acts more like a hormone with multiple effects on different organs than a simple vitamin. Of importance, it regulates the renin-angiotensin system and the immune system, both of which are critical determinants of the severity of the body’s response to Covid-19. Vitamin D reins in inflammatory responses and reduces the cytokine storm that contributes to severe outcomes.
Levels of vitamin D above 35 to 40 ng/mL appear to be best for optimal protection. Most Americans, unfortunately, have levels below 35 ng/mL and would benefit from taking a vitamin D supplement. The situation is even worse with diabetes. A 2012 report in Diabetic Medicine reviewed vitamin D blood levels in adults over 40 collected between 2001 and 2004 in a National Health and Nutrition Examination Survey. They found that 81% of U.S adults aged 40 and older with diabetes have vitamin D levels below 30 ng/mL, the lower limit for normal. Low vitamin D levels were more common among Hispanic Americans (92%) and African Americans (98%) than Anglo Americans (76%).
Does your vitamin D level affect Covid? At the University of Chicago, 489 patients had their vitamin D level measured in the year before being tested for Covid-19. Researchers found people deficient in vitamin D were 1.8 times as likely to test positive for Covid-19 than those with adequate vitamin D. Higher vitamin D levels appear to protect against contracting Covid.
How much vitamin D does a person need when they are deficient? It takes about 5,000 units a day for 3 to 4 months, equivalent to 600,000 units over time, to achieve a reasonable blood level. Afterward, about 2,000 units a day are typically required to maintain that level. Because it is stored in fat cells, larger doses of vitamin D are required for higher BMI people.
But an active form of D called calcifediol (Calcitriol), available by prescription, works faster. In a double-blind study, an experimental group admitted for Covid to a hospital in Spain received 0.532 mg of the prescription medication calcifediol (Calcitriol, equivalent to 100,000 units of vitamin D3) on their first day in the hospital, 0.266 mg (another 50,000 units) on the third and seventh days, and then 50,000 units weekly until discharge or admission to the ICU. A control group received the same standard Covid protocol but not the calcifediol.
Of 76 consecutive patients hospitalized with Covid-19, only 1 of the 50 patients (2%) treated with calcifediol required admission to the hospital’s ICU. In comparison, 13 of the 26 untreated patients (50 %) required ICU admission (p < 0.001). None of the calcifediol-treated patients died, while 2 of the untreated patients died.
For any of the interventions mentioned in our newsletter, there will be studies that show no benefit and those that show benefit, but rarely any that show harm. As an example of one with no benefit, a JAMA paper published this month provided results from a Brazilian study with 120 people in the intervention group and 120 people given a placebo. The researchers found that when researchers gave a single dose of 200,000 vitamin D units to these hospitalized patients, the vitamin did not shorten the number of days they spent in the hospital. However, they gave these patients this dose only after they had had Covid-19 symptoms for an average of more than 10 days. The OTC form of vitamin D3 used in this study requires several modifications internally to transform into its active form like Calcitriol. As ill as these individuals were, these transformations may not have been possible.
In contrast, a 2014 study in Critical Care summarized data from seven well-conducted studies involving 4,204 hospitalized individuals. Of these, 1,679 people were deficient in vitamin D with levels below 10, 12, or 20 ng/ml, depending on the study. Due to softening of the bones, rickets, or bowing of the knees, begins at levels below about 12 ng/ml. Those deficient in vitamin D had a 76% greater chance of dying in the hospital.
If you do not know your current vitamin D level, discuss getting this lab test with your physician. Also, discuss starting on calcifediol that acts more quickly at the first sign of Covid symptoms.
Lots more information and research, with links, can be found on our Vitamin D and COVID-19 page. - Famotidine (Versus Proton-Pump Inhibitors) Famotidine (Pepcid) is an over-the-counter histamine-2 blocker that lowers histamine production. This reduces gastric acid secretion and acid indigestion. It competes with proton-pump inhibitors (PPIs) that directly lower gastric acid levels and are among the world’s most widely used medications. PPIs include medications like Nexium (esomeprazole), Prilosec (omeprazole), Prevacid (lansoprazole), and a dozen other names. Both histamine-2 blockers and PPIs efficiently fight heartburn and Barrett’s esophagitis by lowering gastric acid production in the stomach.
However, gastric acid kills Covid-19 in the stomach. PPIs often reduce the stomach’s acidity to such a degree that the Covid-19 virus passes more easily through the stomach to access a prime target, the cells in the intestines. Like lung cells, intestinal cells have multiple ACE-2 enzyme receptors on their outer walls, which Covid prefers for cell entry.
Researchers recommend famotidine during a pandemic because it does not reduce gastric acidity to the same degree as PPIs.
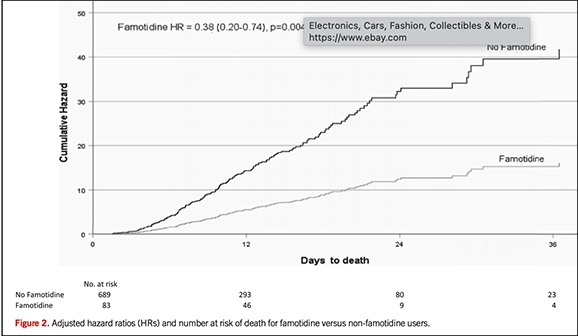
Even better, famotidine directly counters Covid-19 inside cells by blocking the 3-chymotrypsin-like protease enzyme. This blockage lessens Covid’s ability to multiply once it breaks into a human cell. Additionally, it lowers histamine levels that may worsen Covid’s impact. One research study found that famotidine decreased mortality by about 50%, possibly because it leaves more gastric acid in the stomach to kill Covid viruses.
In contrast, a Korean study showed that taking a PPI nearly doubled the severity of Covid-19 infections. Similarly, a survey of over 53,000 people in the U.S. found the risk of getting Covid was 2.1 and 3.7 times higher in those who took a PPI once or twice a day, respectively. Stopping a PPI must be done carefully, so discuss this with your physician before you do anything.
How much famotidine is a good dose to take? For adults at risk for Covid, a 20 mg tablet taken once a day may provide protection even if they have no intestinal problems. If active Covid symptoms begin, higher famotidine doses of 40 to 60 mg taken three times a day appear to reduce both the severity and mortality of Covid-19.
Lots more information and research, with links, can be found on our Pepcid vs. Proton-Pump Inhibitors. - Zinc with quercetin reduces Covid entry into cells, cuts down on its ability to multiply by inhibiting the RNA polymerase enzyme, improves immune responses, and may also lessen the loss of taste and smell during a Covid infection. In the spring of 2020, Spanish researchers reviewed the plasma zinc levels of 249 patients on admission to a hospital with Covid-19. The average plasma zinc level on arrival was 61 mcg/dL. The initial zinc level for the 21 patients (8%) who died from Covid averaged just 43 mcg/dL compared to 63 mcg/dL for those who survived.
People with plasma zinc below 50 mcg/dL at admission were 2.3 times more likely to die in the hospital (p = 0.034) than those with a plasma zinc level of 50 mcg/dL higher. Each mcg/dL increase in plasma zinc at admission was associated with a 7% lower risk of dying in the hospital. (p = 0·0049). Higher zinc levels reduced inflammation at the active infection peak as measured by an inflammatory marker called interleukin-6.
What doses of zinc and quercetin should you take? With a suspected or proven infection, doses of 25 or 50 mg chelated (protein-bound) zinc along with a 500 mg quercetin tablet taken twice a day improves zinc transport into cells. Take with food for less GI irritation.
Lots more information and research, with links, can be found on our Zinc with Quercetin page. - Vitamin C is an essential Covid-19 fighter. Levels of the water-soluble frontline antioxidant vitamin C become rapidly depleted during severe viral infections. Keeping vitamin C levels high provides nearby cells as immune cells release large quantities of free radical oxidants to kill viruses and bacteria.
Vitamin C minimizes damage to nearby cells and organs by countering this friendly fire of free radicals. This protection is essential for heart and brain cells that require high oxygen levels and produce more free radicals themselves.
Vitamin C’s absorption is restricted by the limited number of specialized intestinal cells required for transport into the bloodstream. The intestine can absorb only a few hundred milligrams of vitamin C at a time. Optimal protection with vitamin C requires 4,000 to 6,000 mg spread throughout the day as soon as symptoms suggest a Covid-19 infection. Continue until symptoms fully resolve. Absorption is improved when 6,000 mg of vitamin C powder are mixed into a large glass of water and sipped throughout the day during an active infection. Consuming vitamin C throughout the day maintains vitamin C levels, improves antioxidant protection, and enhances immune responses.
An alternate way to ensure adequate vitamin C absorption utilizes liposomal vitamin C capsules or liquid. Liposomal C has a layer of fat surrounding vitamin C molecules that enables more vitamin C to move through the intestinal wall into the bloodstream. To increase vitamin C levels during severe infection, take a 1,500 mg dose of liposomal vitamin C three times a day or 1,000 mg four times a day. Continue until symptoms fully resolve. Both vitamin C powder and liposomal vitamin C are over-the-counter.
Lots more information and research, with links, can be found on our Vitamin C and COVID-19 page. - Januvia or berberine Covid-19 enters cells through at least two cell surface enzymes. To enter cells, Covid uses its spike protein to attach to angiotensin-converting enzyme-2 (ACE-2) receptors and also to dipeptidyl peptidase-4 (DPP-4) enzyme receptors on cell walls. One study revealed that blocking DPP-4 receptors with Januvia significantly reduced Covid-19 death rates by more than half and improved clinical outcomes.
A prescription for 100 mg BID of Januvia at diagnosis or onset of symptoms may help. Because of how it works, Januvia does not cause hypoglycemia and may protect regardless of diabetes. Berberine, a compound found in goldenseal and tree turmeric, is used for diabetes, and like Januvia, blocks the DPP-4 enzyme. Furthermore, berberine lessens viral multiplications, regulates viral signaling pathways, and supports host immune responses to improve viral clearance.
Lots more information and research, with links, can be found on our Januvia, Berberine, and Covid-19 page.
Before getting Covid, take all diabetes medications as usual. However, if you get Covid, you want to know which diabetes medications to continue and when to stop. These are current recommendations.
- Always continue your insulin. Much higher doses of this critical medication are often required to control glucose levels during Covid-19 infections. Covid can directly damage the beta cells that make insulin. This creates a high risk for DKA in Type 1 diabetes, Type 2 diabetes, and even people with no prior history of diabetes.
- Continue DPP-4 inhibitors like Januvia, Tradjenta, and Onglyza. In an early study, Januvia appears to reduce mortality during Covid. Other DPP-4 inhibitors may do the same.
If nausea, vomiting, or diarrhea begins:
- Stop sodium-glucose cotransporter-2 inhibitors (SGLT-2 inhibitors) like Invokana (canagliflozin), Farxiga (dapagliflozin), and Jardience (empagliflozin). SGLT-2s carry a higher risk for DKA and dehydration. It can also mask DKA by keeping glucose levels relatively low even as DKA develops. Talk with your physician about stopping an SGLT-2 at the first sign of a Covid-19 infection.
- Stop metformin. Metformin carries increased risks for dehydration from its side effects of nausea, vomiting, diarrhea, and lactic acidosis. These typically minimal risks become dangerous when combined with the high risk for diabetic ketoacidosis (DKA) carried by Covid.
- Stop GLP-1 medications like Trulicity and Ozempic. GLP-1s may trigger nausea, vomiting, or diarrhea. These risks become greater when combined with the high risk of DKA with Covid.
Continue sulfonylureas and meglitinides unless glucose tests show a risk of hypoglycemia.

 Researchers recommend famotidine during a pandemic because it does not reduce gastric acidity to the same degree as PPIs.
Researchers recommend famotidine during a pandemic because it does not reduce gastric acidity to the same degree as PPIs.