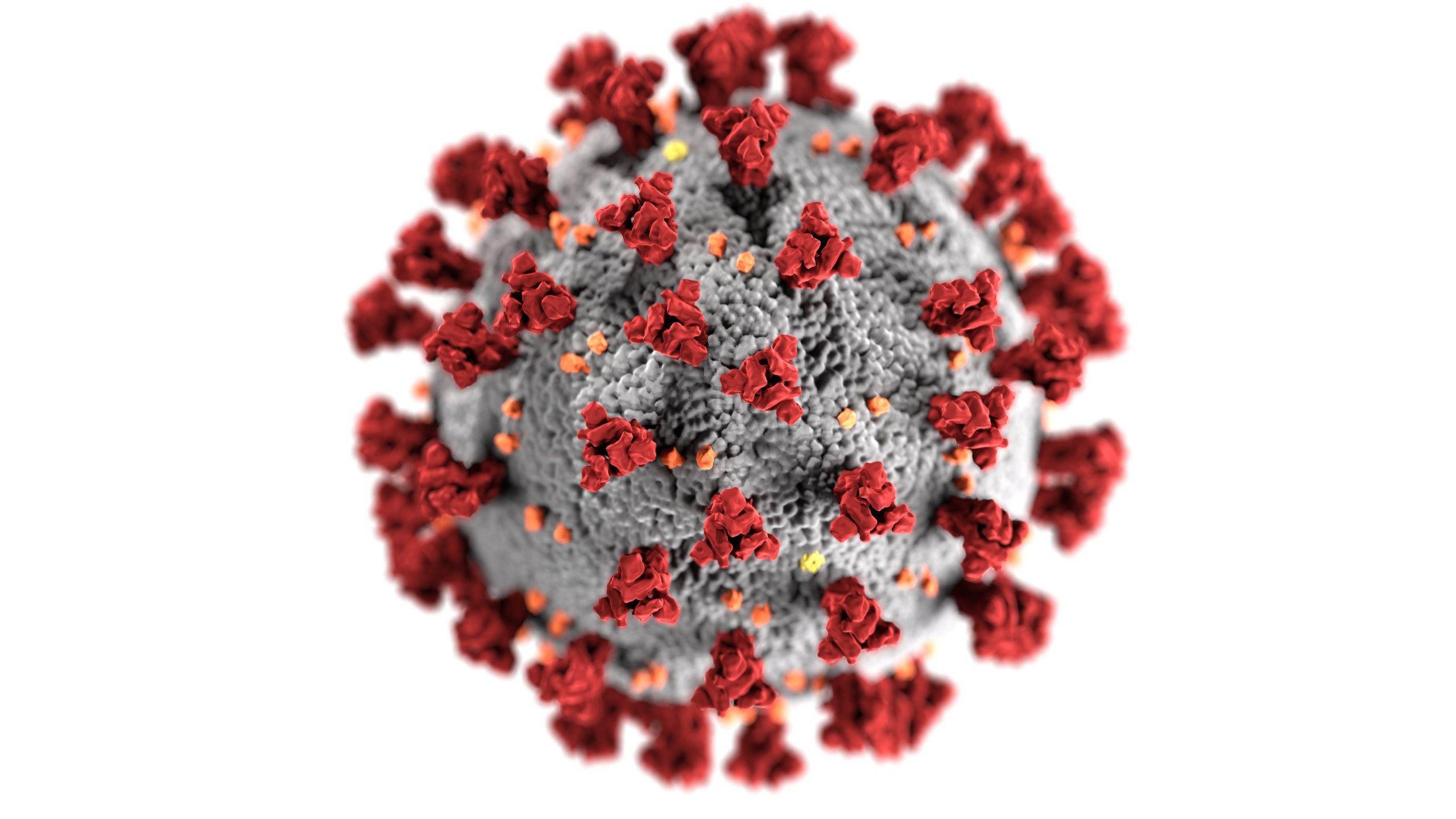
Covid-19 is not the flu. Covid-19 (COrona VIrus Disease-2019), the Severe Acute Respiratory Syndrome CoronaVirus 2 (SARS-CoV-2), started in 2019. The Corona name arises from the multiple “spike” proteins on the virus’s outer shell that resemble a crown or corona. Covid-19 uses its spike proteins like a crowbar to break into a cell, hijack the cell’s enzymes and materials to make multiple copies of itself, and kill the cell.
COVID-19, a single-stranded RNA, is not alive but relies on infecting a host to survive. It is one-tenth of a micron or about one-tenth of the size of common bacteria. Despite its tiny size and the milder infections it sometimes causes, COVID-19 can turn deadly when it takes over many of the body’s cell operations. The virus uses as many as 300 human proteins and enzymes to make multiple copies of its RNA and protective fatty exterior. It also manufactures a bubble enclosure that allows it to exit the cell. Using normal cell functions, COVID continues its attack and exponentially increases the infection.
COVID-19 has structural similarities to other viruses we’ve seen before, with differences. Four earlier Coronavirus infections appeared as common colds, along with two more deadly versions. The 2002 through 2004 severe acute respiratory syndrome [SARS-CoV] was far more lethal than COVID-19, killing 11 of every 100 people who got it. However, by luck, it happened to be less contagious. In total, it killed fewer than 1,000 people.
In 2012, the Middle East respiratory syndrome [MERS-CoV] spread from infected camels to people in Saudi Arabia. It killed 35%, more than one of every three people who got it. Although occasional cases still occur today, total mortality remains below 900 individuals. MERS, again, fortunately, was hard to spread.
Viruses become pandemics once they combine ease of transmission with high mortality rates. COVID-19 shares the ease of spread of its cold virus cousins, along with a higher mortality rate like SARS-CoV, although it is substantially below SARS. Of concern, scientists have never developed a successful vaccine against a cold or the SARS virus.
In 2014, the unrelated Ebola virus broke out in Africa. If these or similar viruses mutated and became contagious, the potential for high mortality rates prompted President Obama to have the NIH develop a pandemic plan for this country. This plan enhanced federal responses and began to build a public health infrastructure for the predicted pandemics. The NIH pandemic plan, developed and later presented to the Trump administration, along with clear directions for handling COVID-19, was ignored. The excessive death toll in the U.S. is a direct result of delays in testing, monitoring, face mask production, social distancing, hand washing, and contact tracing.
As of June 2, 2020, less than 0.65%, or one out of every 150 people in the U.S. population, has contracted COVID-19. Unfortunately and needlessly, over 120,000 people have already died. To acquire herd immunity, 70% of the U.S. population needs to become infected. The CDC projects 140,000 deaths in the U.S. by July 1, 2020. The 1918 H1N1 flu pandemic killed 675,000 people in this country. If no significant intervention becomes viable, over 2,000 participants’ average projections suggest that worldwide COVID deaths will reach 2 million by January 1, 2021. Ten to 15% of all cases require hospitalization. Hospitals, mortuaries, and graveyards will need significant modifications to prepare for this.
A report regarding 1,150 COVID-19 positive patients admitted to New York hospitals during March 2019 found that 17% of those hospitalized required intubation and ventilation. Some 80% of those admitted to an ICU required ventilation to stay alive. Men have more ACE2 enzyme receptors than women, so it is not surprising that two out of three ICU patients are men. Among those hospitalized, at least one out of seven requires dialysis while there. In the months and years following hospitalization, a significant number of people face prolonged or lifelong conditions like decreased lung capacity, advanced cardiovascular disease, or need for dialysis at a younger age.
Never compare COVID-19 to the flu. Never treat it like one.
Last Updated on July 15, 2025